Life Saving Priorities: Capacity Building
Originally posted on the CCBRT blog
Tanzania is home to seven health professionals per 10,000 population. The World Health Organization recommends 45 per the same number of people. This workforce shortage overwhelms health professionals, leading to poor working conditions, poor quality of care and poor health outcomes. Facing these challenges, how does Kupona’s partner in Tanzania, CCBRT, save lives? By prioritizing capacity building.
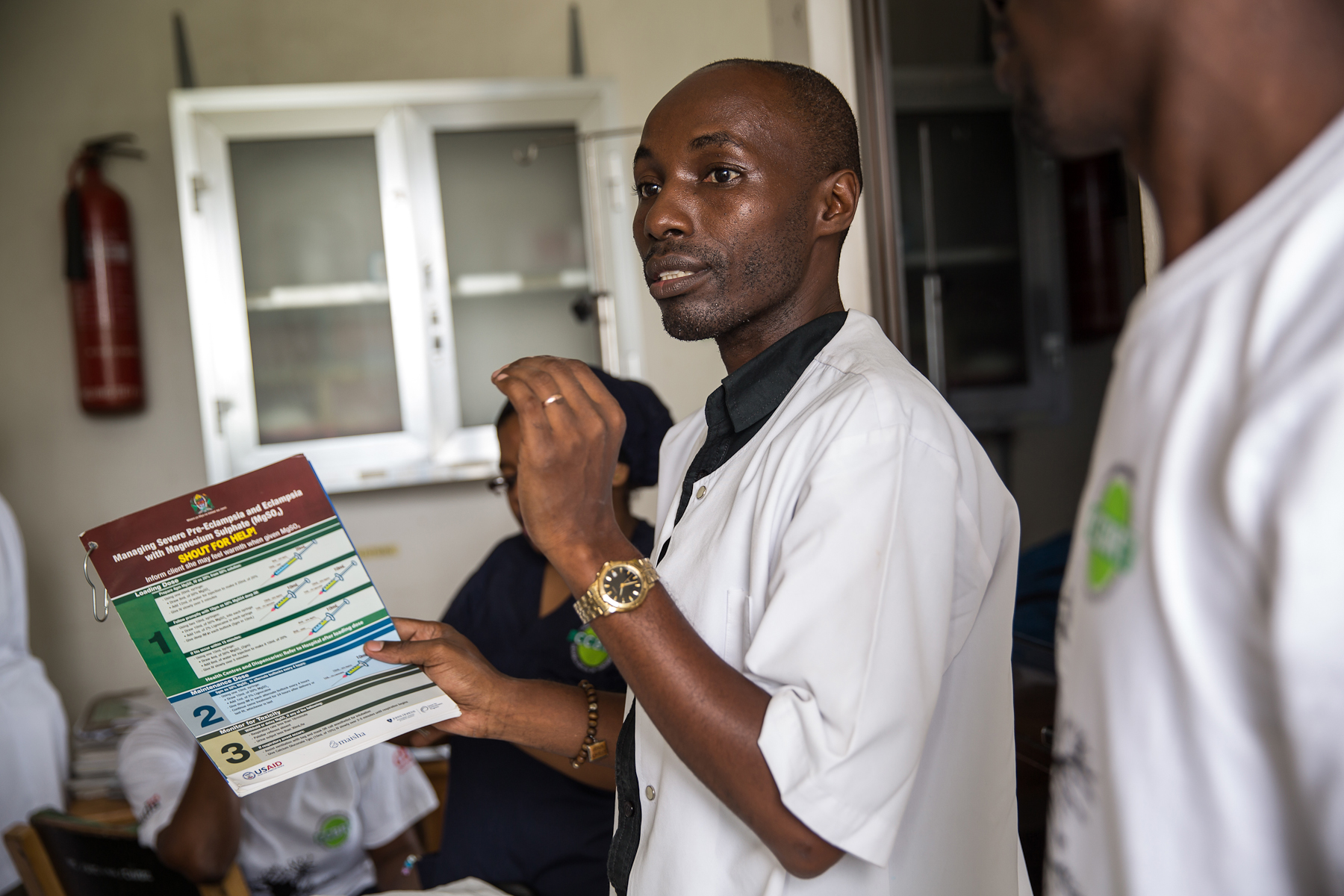
Capacity building can take many shapes and forms. It can focus on the needs of CCBRT, like sponsored trainings for doctors to specialize in anesthesiology. It can focus on the needs of partner facilities, like newborn health equipment donated to Temeke Hospital. Or it can focus on the needs of the greater Tanzanian health workforce, like planning for the CCBRT Centre for Excellence in Clinical Education.
Perhaps the greatest example of CCBRT’s efforts in the past five years lies in their Maternal & Newborn Health Capacity Building (MHCB) Program, currently working in 23 sites across Dar es Salaam. MHCB aims to strengthen the skills of health professionals to improve health outcomes for mothers and babies. From 2013 to 2017, this included training, coaching and mentoring of more than 5,000 healthcare workers.
The results for health services? An increase in the use of life saving interventions, like vacuum delivery (used when labor has not progressed adequately), Cesarean section (used when vaginal delivery would risk the life of mother or baby) and Kangaroo Mother Care (used when a baby is born premature).
The results for quality of care? A 720% increase – from 10% to 82% – in quality of care, according to standards-based performance assessments. These measure adherence to standards related to labor, delivery and newborn care, infrastructure, human resources, education, communication and support systems.
And the results for patients? As of 2016, a 40% reduction in maternal deaths and a 14% reduction in stillbirths across facilities – with further reductions expected in 2017.
As one nurse reported, “If I can now save children, it is only because of what I have learned from CCBRT. Before I was not fully aware of what to do, for example, with premature kids, but now it is a pleasure for me to see them grow through Kangaroo Mother Care!”
A new mother of twins echoed this statement: “I was scared, as I had never experienced premature babies. But doctors and nurses advised on taking care of them. I am grateful for their help because, without it, I would have lost them.”
Providers and patients agree: the MHCB model works. The achievements of this program from 2013 to 2017 pave the way for additional activities in the upcoming strategy period, from 2018 to 2022. Following the success of supporting frontline health workers, the next phase of capacity building will support leaders in the regional health system.